|

HOME |
ABOUT | INDEX |
NEWS |
FACEBOOK |
CONTACT
SAFE
SEX
Protection | Sexually Transmitted Infection

Health and Medical Issues
AIDS|HIV
Physical and Sexual
Sensual and Seductive
Relationships|Couples
Dating
Defining Safe Sex
Safe sex is sexual
activity engaged in by people who have taken precautions
to protect themselves against sexually transmitted
infections (STIs) or sexually transmitted diseases
(STDs) such as HIV. It is also referred to as safer sex
or protected sex, while unsafe or unprotected sex is
sexual activity engaged in without precautions,
especially forgoing condom use. Some sources prefer the
term safer sex to more precisely reflect the fact that
these practices reduce, but do not always completely
eliminate, the risk of disease transmission.
 Safe sex practices became
more prominent in the late 1980s as a result of the AIDS
epidemic. Promoting safe sex is now one of the aims of
sex education. Safe sex is regarded as a harm reduction
strategy aimed at reducing risks. The risk reduction of
safe sex is not absolute; for example, the reduced risk
to the receptive partner of acquiring HIV from HIV-seropositive
partners not wearing condoms compared to when they wear
them is estimated to be about a four to fivefold.
Although some safe sex
practices can be used as birth control (contraception),
most forms of contraception do not protect against STIs
(or STDs). Likewise, some safe sex practices, like
partner selection and low-risk sex behavior, are not
effective forms of contraception but should be
considered before engaging in any form of intercourse to
reduce risk.
WebMD:
Preventing STDs with Safe Sex
HIV
Equal: 7 Different Ways to Have Safe Sex
Info: Health and Medical Concerns
Better Health: Safe Sex
How to Talk to Your Partners About STIs, According to
Queer Experts
Safe sex practices became
more prominent in the late 1980s as a result of the AIDS
epidemic. Promoting safe sex is now one of the aims of
sex education. Safe sex is regarded as a harm reduction
strategy aimed at reducing risks. The risk reduction of
safe sex is not absolute; for example, the reduced risk
to the receptive partner of acquiring HIV from HIV-seropositive
partners not wearing condoms compared to when they wear
them is estimated to be about a four to fivefold.
Although some safe sex
practices can be used as birth control (contraception),
most forms of contraception do not protect against STIs
(or STDs). Likewise, some safe sex practices, like
partner selection and low-risk sex behavior, are not
effective forms of contraception but should be
considered before engaging in any form of intercourse to
reduce risk.
WebMD:
Preventing STDs with Safe Sex
HIV
Equal: 7 Different Ways to Have Safe Sex
Info: Health and Medical Concerns
Better Health: Safe Sex
How to Talk to Your Partners About STIs, According to
Queer Experts
Info: Sexual Activity
Tips for Dating When Youíre HIV Positive
Naked Truth: Sex Can Be Infectious
WebMD Slideshow: Cleaning Up After Sex
 Highest STI Rates in the US
These 50 cities have the highest STI rates in the US
Highest STI Rates in the US
These 50 cities have the highest STI rates in the US
A new analysis of data from the CDC has produced a list
of the 50 metropolitan areas with the highest STI rates
in the US. As weíve reported before, STI rates
have continued to increase over the last decade. While
HIV transmission has eased somewhat, rates of chlamydia,
gonorrhea and syphilis have rocketed. Gay men are
disproportionately impacted. In 2022, across the
US, around 1 in 130 people were diagnosed with an STI.
However, thatís the average. In some locations, the
number was far greater.
The worst place for STIs, perhaps surprisingly is
Philadelphia. One in 65 residents were diagnosed with an
infection in 2022 in the city of brotherly love. This
was followed by Memphis (TN), Jackson (MI) and New
Orleans, LA. St. Louis (MO), rounded off the top five.
In terms of gay hotspots, San Francisco (CA) came in
eighth place.
If you want to move somewhere with low STD rates,
placing 100th in the ranking is Provo, Utah. The city
has a high Mormon population, and only 300 out of every
100,000 residents were diagnosed with an STD (well below
the 751 average or the 1,504 per 100k in Philadelphia).

Oraquick: The Musical
Queer Artists Changing Our
View of Sexual Health
Fabulous Approach to Promoting LGBTQ Health
Planned Parenthood: Safer Sex
Condoms and Birth Control
Tips for Dating When Youíre HIV Positive
How to Talk to Your Partners About STIs, According to
Queer Experts
WebMD Slideshow: Cleaning Up After Sex
Condoms and Birth Control
The top 50 cities (with case numbers per 100,000
residents) is as follows...
|
Philadelphia, PA (1,504)
Memphis, TN (1,498)
Jackson, MS (1,490)
New Orleans, LA (1,450)
St. Louis, MO (1,423)
Baton Rouge, LA (1,332)
Montgomery, AL (1,323)
San Francisco, CA (1,285)
Detroit, MI (1,267)
Washington, DC (1,266)
Little Rock, AR (1,252)
Norfolk, VA (1,252)
Portland, OR (1,244)
Mobile, AL (1,234)
Cleveland, OH (1,228)
Miami, FL (1,221)
Minneapolis, MN (1,201)
Laredo, TX (1,184)
San Antonio, TX (1,178)
Milwaukee, WI (1,172)
Columbia, SC (1,166)
Richmond, VA (1,154)
Fort
Lauderdale, FL (1,100)
Lexington, KY (1,068)
Augusta, GA (1,060)
 |
Tampa,
FL (1,060)
Nashville, TN (1,045)
Charlotte, NC (1,044)
Oakland, CA (1,027)
Corpus Christi, TX (1,019)
Knoxville, TN (1,009)
Indianapolis, IN (1,003)
Greensboro, NC (1,002)
Orlando, FL (1,000)
Tucson, AZ (996)
New York, NY (979)
Atlanta, GA (977)
Phoenix, AZ (970)
Austin, TX (969)
Albuquerque, NM (959)
Bakersfield, CA (953)
Kansas City, MO (952)
Des Moines, IA (942)
Houston, TX (940)
Los Angeles, CA (924)
Fresno, CA (918)
Oklahoma, OK (900)
Toledo, OH (889)
Wichita, KS (864)
Dallas, TX (861)
 |
The
southern states are disproportionately represented.
Seventeen of the top 25 cities are in the south. This
trend has previously been noted in regard to HIV
transmission.
Baltimore
is missing from the list. The previous year, it ranked
no. 4 on this list. Data was not available for Baltimore
for this recent study.
STI rates dipped in 2020 because of the Covid pandemic.
However, the 2022 figures showed a return to pre-Covid
levels. There were 710,000 new cases of gonorrhea, and
1.6 million of chlamydia, while syphilis rates have
risen by 28.6 percent in just a year.
Gay men are advised to have a sexual health check-up at
least once a year, regardless of whether they have any
symptoms. If you have multiple partners, get tested once
every three months.
[Source:
Centers for Disease Control & Prevention, May 2024]
WebMD:
Preventing STDs with Safe Sex
Info: Health and Medical Concerns
HIV
Equal: 7 Different Ways to Have Safe Sex
Info: AIDS/HIV
Better Health: Safe Sex
Info: Sexual Activity
Naked Truth: Sex Can Be Infectious
Questions About HIV You've Been Afraid to Ask
 CDC
Report: Top Three STDs
Nearly 2.3
million cases of chlamydia, gonorrhea, and syphilis were
diagnosed in the United States in 2017, according to
preliminary data released by the Centers for Disease
Control & Prevention (CDC) at the National STD
Prevention Conference in Washington, DC.
CDC
Report: Top Three STDs
Nearly 2.3
million cases of chlamydia, gonorrhea, and syphilis were
diagnosed in the United States in 2017, according to
preliminary data released by the Centers for Disease
Control & Prevention (CDC) at the National STD
Prevention Conference in Washington, DC.
Chlamydia,
gonorrhea, and syphilis are curable with antibiotics,
yet most cases go undiagnosed and untreated ó which can
lead to severe adverse health effects that include
infertility, ectopic pregnancy, stillbirth in infants,
and increased HIV risk. Prior studies suggest a range of
factors may contribute to STD increases, including
socioeconomic factors like poverty, stigma, and
discrimination; and drug use.
[Source:
Centers for Disease Control & Prevention, September
2018]
CDC Press Release: Steep Increase in STDs
CDC Help: What To Do If You Test Positive for Gonorrhea
or Chlamydia
CDC Info:
What Are STDs?
Safe Sex Information
Safe sex is all about
protecting yourself and your partners from sexually
transmitted infections. Safe sex helps you stay healthy
and can even make sex better.
STDs are infections that
are passed from one person to another during sexual
activity. Anybody who has oral, anal, or vaginal sex, or
genital skin-to-skin contact with another person can get
STDs. Safe sex means taking steps to protect yourself
and your partner from STDs when you have sex.

Oraquick: The Musical
Queer Artists Changing Our
View of Sexual Health
Fabulous Approach to Promoting LGBTQ Health
Planned Parenthood: Safer Sex
Condoms and Birth Control
Tips for Dating When Youíre HIV Positive
How to Talk to Your Partners About STIs, According to
Queer Experts
WebMD Slideshow: Cleaning Up After Sex
Condoms and Birth Control
There are lots of ways
you can make sex safer. One of the best ways is by using
a barrier (like condoms, female condoms, dental dams)
every single time you have oral, anal, or vaginal sex.
Barriers cover parts of your genitals, protecting you
and your partner from body fluids and some skin-to-skin
contact, which can both spread STDs.
Getting tested for STDs
regularly is also part of safe sex, even if you always
use condoms and feel totally fine. Most people with STDs
donít have symptoms or know theyíre infected, and they
can easily pass the infection to their partners. So
testing is the only way to know for sure whether or not
someone has an STD.
Getting tested protects
you by letting you know if you DO have an STD, so you
can get the right treatment to stay healthy and avoid
giving it to other people.

 Sticking to sexual
activities that donít spread STDs (like outercourse or
mutual masturbation) is a great way to safely get sexual
pleasure and be intimate with another person. But if
youíre taking off underwear and touching each other or
having any kind of sex, using barriers is the safer way
to go.
Another way to make sex
safer is to avoid drinking too much alcohol or doing
other drugs. Getting wasted can make you forget how
important safer sex is, and you may accidentally make
decisions that increase your chances of getting STDs.
Itís also harder to use condoms correctly and remember
other safer sex basics when youíre drunk or high.
The only way to be
totally sure you wonít get an STD is to never have any
kind of sexual contact with another person. But that
doesnít work for the vast majority of people. Most of us
are sexually intimate with other people at some point in
our lives. So if youíre going to have sex, making it
safe sex is the best way to help you avoid getting or
passing an STD.
[Source: Planned
Parenthood]
Sticking to sexual
activities that donít spread STDs (like outercourse or
mutual masturbation) is a great way to safely get sexual
pleasure and be intimate with another person. But if
youíre taking off underwear and touching each other or
having any kind of sex, using barriers is the safer way
to go.
Another way to make sex
safer is to avoid drinking too much alcohol or doing
other drugs. Getting wasted can make you forget how
important safer sex is, and you may accidentally make
decisions that increase your chances of getting STDs.
Itís also harder to use condoms correctly and remember
other safer sex basics when youíre drunk or high.
The only way to be
totally sure you wonít get an STD is to never have any
kind of sexual contact with another person. But that
doesnít work for the vast majority of people. Most of us
are sexually intimate with other people at some point in
our lives. So if youíre going to have sex, making it
safe sex is the best way to help you avoid getting or
passing an STD.
[Source: Planned
Parenthood]
Planned Parenthood: Safer Sex
Info: AIDS/HIV
WebMD Slideshow: Cleaning Up After Sex
Condoms and Birth Control
Tips for Dating When Youíre HIV Positive
Top STIs and How to Treat and Avoid Them
Wikipedia: Safe Sex Defined
Info: Sexual Activity
WebMD: Understanding STD Prevention
FDA Approves First Condom Specifically
for Anal Sex
 How Do You Get STDs?
STDs are usually passed
from one person to another during oral, anal, or vaginal
sex. There are lots of different STDs. Some are carried
in body fluids like semen, vaginal fluids, and blood.
Others can be passed just from skin-to-skin touching
with an infected body area. Using barriers like condoms
and dams helps you avoid contact with fluids and some
types of skin-to-skin contact during sex. So when you
donít use condoms, your chance of getting an STD goes
up.
How Do You Get STDs?
STDs are usually passed
from one person to another during oral, anal, or vaginal
sex. There are lots of different STDs. Some are carried
in body fluids like semen, vaginal fluids, and blood.
Others can be passed just from skin-to-skin touching
with an infected body area. Using barriers like condoms
and dams helps you avoid contact with fluids and some
types of skin-to-skin contact during sex. So when you
donít use condoms, your chance of getting an STD goes
up.
 All STDs can infect your
genitals. Vaginal or anal sex without a condom has a
high risk for passing:
All STDs can infect your
genitals. Vaginal or anal sex without a condom has a
high risk for passing:
|
--chlamydia
--gonorrhea
--syphilis
--HIV
--herpes

|
--HPV and genital warts
--hepatitis B
--pubic lice
--scabies
--trichomoniasis

|
Some STDs can also infect
your lips, mouth, and throat. Oral sex without a condom
or dam has a high risk for passing: herpes, syphilis, gonorrhea, HPV, hepatitis B.
Some STDs can be passed
even if thereís only some skin on skin action with no
fluids passed. Genital skin-to-skin contact can spread: herpes, HPV, pubic lice, scabies.
[Source: Planned
Parenthood]
 WebMD:
Preventing STDs with Safe Sex
Info: Health and Medical Concerns
HIV
Equal: 7 Different Ways to Have Safe Sex
Info: AIDS/HIV
Better Health: Safe Sex
How to Talk to Your Partners About STIs, According to
Queer Experts
Info: Sexual Activity
Naked Truth: Sex Can Be Infectious
Questions About HIV You've Been Afraid to Ask
Types of Safe Sex Activity
Are some kinds of sex
safer than others? Yes. There are even a few totally
risk-free ways to get sexual pleasure and be intimate
with another person, like masturbating, and dry humping
(grinding) with clothes on.
Low risk activities
include kissing, touching your partnerís genitals with
your hands, using sex toys with a partner, dry humping
(grinding) without clothes, and oral sex. But itís still
possible to get certain STDs from these things, so using
condoms and dams to avoid contact with skin and fluids
whenever you can helps you stay healthy.
WebMD:
Preventing STDs with Safe Sex
Info: Health and Medical Concerns
HIV
Equal: 7 Different Ways to Have Safe Sex
Info: AIDS/HIV
Better Health: Safe Sex
How to Talk to Your Partners About STIs, According to
Queer Experts
Info: Sexual Activity
Naked Truth: Sex Can Be Infectious
Questions About HIV You've Been Afraid to Ask
Types of Safe Sex Activity
Are some kinds of sex
safer than others? Yes. There are even a few totally
risk-free ways to get sexual pleasure and be intimate
with another person, like masturbating, and dry humping
(grinding) with clothes on.
Low risk activities
include kissing, touching your partnerís genitals with
your hands, using sex toys with a partner, dry humping
(grinding) without clothes, and oral sex. But itís still
possible to get certain STDs from these things, so using
condoms and dams to avoid contact with skin and fluids
whenever you can helps you stay healthy.


 Wikipedia: Safe Sex Defined
WebMD:
Preventing STDs with Safe Sex
HIV
Equal: 7 Different Ways to Have Safe Sex
Better Health: Safe Sex
HIV
Equal: 7 Different Ways to Have Safe Sex
Top STIs and How to Treat and Avoid Them
FDA Approves First Condom Specifically
for Anal Sex
Wikipedia: Safe Sex Defined
WebMD:
Preventing STDs with Safe Sex
HIV
Equal: 7 Different Ways to Have Safe Sex
Better Health: Safe Sex
HIV
Equal: 7 Different Ways to Have Safe Sex
Top STIs and How to Treat and Avoid Them
FDA Approves First Condom Specifically
for Anal Sex
US Dept of Health & Human Services: Reducing Risk With
PrEP
Naked Truth: Sex Can Be Infectious
Questions About HIV You've Been Afraid to Ask
Having vaginal or anal
sex without a condom is super risky. You can get any and
all STDs from unprotected vaginal or anal sex. The best
way to protect yourself if youíre going to have vaginal
or anal sex is use a condom every single time. Using
lube with that condom also makes sex safer, especially
anal sex.
When it comes to HIV,
oral sex is much safer sex than vaginal or anal sex. But
other infections, like herpes, syphilis, hepatitis B,
gonorrhea, and HPV, can be passed during oral sex. So no
matter what kind of sex you have, use condoms or dams to
make it safer.
If I have an STD, how can
I have safe sex? If you find out that you have an
STD, itís important to know how to have safe sex and
avoid passing it on. Luckily, many STDs can be easily
cured with medication, so once you finish treatment, you
donít have to worry about giving your STD to anyone.

Planned Parenthood: Safer Sex
WebMD Slideshow: Cleaning Up After Sex
Condoms and Birth Control
Wikipedia: Safe Sex Defined
Info: Sexual Activity
WebMD: Understanding STD Prevention
FDA Approves First Condom Specifically
for Anal Sex
And even though some STDs
canít be cured, there are ways to treat your symptoms
and help avoid giving your STD to people you have sex
with. Depending on what STD you have, there are things
you can do to protect your partners. Hereís a handy
checklist:
--Always use condoms and
dental dams during oral, anal, and vaginal sex ó whether
or not you have an STD.
--Donít have sex at all
if you have any STD symptoms (like sores or warts around
your genitals, weird discharge from your penis, vagina
or anus, or itching, pain, irritation and/or swelling in
your penis, vagina, vulva, or anus).
--Go see a doctor or
nurse so they can start treating your STD as soon as
possible.
 --If you have a curable
STD (like gonorrhea, chlamydia, or syphilis), take all
of your medication the way your doctor tells you to,
even if your symptoms go away sooner. The infection
stays in your body until you totally finish the
treatment. Your partner(s) should also be treated at the
same time. Donít have sex at all until you both finish
your treatment, and your doctor or nurse says itís OK.
--If you have an STD that
canít be cured (like HIV or herpes), talk with your
doctor about medicines that can help lower your chances
of spreading it to a partner. Depending on what STD you
have and where it is, you may need to use condoms/dams
every time you have oral, anal, and/or vaginal sex.
--Always tell your sexual
partners that you have an STD before you have sex, so
you can work together to make a safe sex plan and help
prevent it from spreading. Itís not the easiest
conversation, but itís an important one.
[Source: Planned
Parenthood]
--If you have a curable
STD (like gonorrhea, chlamydia, or syphilis), take all
of your medication the way your doctor tells you to,
even if your symptoms go away sooner. The infection
stays in your body until you totally finish the
treatment. Your partner(s) should also be treated at the
same time. Donít have sex at all until you both finish
your treatment, and your doctor or nurse says itís OK.
--If you have an STD that
canít be cured (like HIV or herpes), talk with your
doctor about medicines that can help lower your chances
of spreading it to a partner. Depending on what STD you
have and where it is, you may need to use condoms/dams
every time you have oral, anal, and/or vaginal sex.
--Always tell your sexual
partners that you have an STD before you have sex, so
you can work together to make a safe sex plan and help
prevent it from spreading. Itís not the easiest
conversation, but itís an important one.
[Source: Planned
Parenthood]
Planned Parenthood: Safer Sex
Info: AIDS/HIV
How to Talk to Your Partners About STIs, According to
Queer Experts
Condoms and Birth Control
Tips for Dating When Youíre HIV Positive
Wikipedia: Safe Sex Defined
Top STIs and How to Treat and Avoid Them
WebMD:
Preventing STDs with Safe Sex
HIV
Equal: 7 Different Ways to Have Safe Sex
Better Health: Safe Sex
 Outercourse vs. Intercourse
Outercourse is other sexual activities besides vaginal
sex. Sexual abstinence and outercourse can mean
different things to different people.
Outercourse vs. Intercourse
Outercourse is other sexual activities besides vaginal
sex. Sexual abstinence and outercourse can mean
different things to different people.
Non-penetrative sex or outercourse is sexual activity
that usually does not include sexual penetration. It
generally excludes the penetrative aspects of vaginal,
anal, or oral sexual activity, but includes various
forms of sexual and non-sexual activity, such as
frottage, mutual masturbation, kissing, or cuddling.
Some forms of non-penetrative sex, particularly when
termed outercourse, include penetrative aspects, such as
penetration that may result from forms of fingering or
oral sex.
People engage in non-penetrative sex for a variety of
reasons, including as a form of foreplay or as a primary
or preferred sexual act. Heterosexual couples may engage
in non-penetrative sex as an alternative to
penile-vaginal penetration, to preserve virginity, or as
a type of birth control. Same-sex couples may also
engage in non-penetrative sex to preserve virginity,
with gay males using it as an alternative to anal
penetration.
Although sexually transmitted infections (STIs/STDs)
such as herpes, HPV, and pubic lice can be transmitted
through non-penetrative genital-genital or genital-body
sexual activity, non-penetrative sex may be used as a
form of safer sex because it is less likely that body
fluids (the main source of STI/STD transmission) will be
exchanged during the activities, especially with regard
to aspects that are exclusively non-penetrative.
Abstinence and Outercourse
Overview of Outercourse Sexual Activity
Outercourse Techniques
Questions About Outercourse
Outercourse: Non-Penetrative Sex
 Pre-Exposure Prophylaxis
Pre-exposure prophylaxis, or PrEP, is a way for people
who do not have HIV but who are at substantial risk of
getting it to prevent HIV infection by taking a pill
every day. The pill (brand name Truvada or Descovy)) contains two
medicines (tenofovir and emtricitabine) that are used in
combination with other medicines to treat HIV. When
someone is exposed to HIV through sex or injection drug
use, these medicines can work to keep the virus from
establishing a permanent infection.
Pre-Exposure Prophylaxis
Pre-exposure prophylaxis, or PrEP, is a way for people
who do not have HIV but who are at substantial risk of
getting it to prevent HIV infection by taking a pill
every day. The pill (brand name Truvada or Descovy)) contains two
medicines (tenofovir and emtricitabine) that are used in
combination with other medicines to treat HIV. When
someone is exposed to HIV through sex or injection drug
use, these medicines can work to keep the virus from
establishing a permanent infection.
When taken consistently, PrEP has been shown to reduce
the risk of HIV infection in people who are at high risk
by up to 92%. PrEP is much less effective if it is not
taken consistently.
PrEP is a powerful HIV prevention tool and can be
combined with condoms and other prevention methods to
provide even greater protection than when used alone.
But people who use PrEP must commit to taking the drug
every day and seeing their health care provider for
follow-up every 3 months. Truvada and Descovy are
manufactured by Gilead Sciences.
Descovy for PrEP
CDC: Pre-Exposure Prophylaxis
Facts and Info:
What is PrEP?
US Dept of Health & Human Services: Reducing Risk With
PrEP
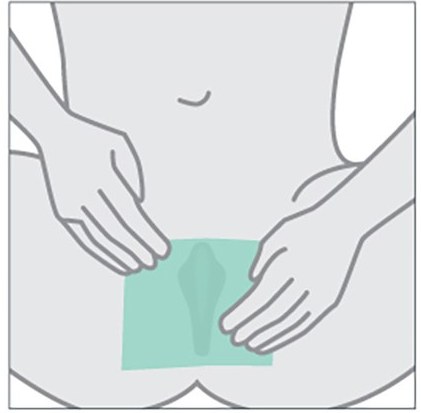
 Dental Dams
Dental dams are for use during
cunnilingus and anilingus, especially for women who have
sex with women. After lubrication with a water-based
lubricant, an unpunctured dental dam may be held over
the vulva or anus, allowing oral stimulation of these
areas without transmission of bodily fluids and direct
physical contact. Condoms can be turned into dental dams
if they are properly cut.
A dental dam, like a condom, is a barrier
method. It is a thin, square piece of rubber which is
placed over the labia or anus during oral-vaginal or
oral-anal intercourse.
Dental dams are most often made of thin
latex or silicone. Although specially-made rubber dental
dams are sold in stores, clear plastic wrap from your
kitchen can serve as an effective dental dam as well. A
dental dam can help reduce the risk of STD transmission,
including herpes, genital warts (HPV), and HIV.
Dental Dams
Dental dams are for use during
cunnilingus and anilingus, especially for women who have
sex with women. After lubrication with a water-based
lubricant, an unpunctured dental dam may be held over
the vulva or anus, allowing oral stimulation of these
areas without transmission of bodily fluids and direct
physical contact. Condoms can be turned into dental dams
if they are properly cut.
A dental dam, like a condom, is a barrier
method. It is a thin, square piece of rubber which is
placed over the labia or anus during oral-vaginal or
oral-anal intercourse.
Dental dams are most often made of thin
latex or silicone. Although specially-made rubber dental
dams are sold in stores, clear plastic wrap from your
kitchen can serve as an effective dental dam as well. A
dental dam can help reduce the risk of STD transmission,
including herpes, genital warts (HPV), and HIV.


 Queer Girls, Dental Dams, and STIs
CDC: How to Use a Dental Dam
Queer Girls, Dental Dams, and STIs
CDC: How to Use a Dental Dam
HOME
QUEER CAFE
│ LGBTQ Information Network │ Established 2017 |